Living with epilepsy brings a myriad of challenges, with the unpredictability of seizures impacting every aspect of daily life. However, a transformative solution has emerged in the form of Vagus Nerve Stimulation (VNS) therapy, changing the game for individuals seeking effective seizure control. In this comprehensive guide, we explore the profound effects of VNS therapy and how it is reshaping the landscape of epilepsy treatment.
How Does VNS Work?
VNS involves the implantation of a device called a vagus nerve stimulator, which is usually placed under the skin on the chest. The device is connected to a wire that is threaded under the skin and attached to the left vagus nerve in the neck.
The vagus nerve is a major nerve that connects the brain to various parts of the body. VNS works by delivering regular, mild electrical pulses to the brain through the vagus nerve. It is believed that these electrical impulses can help prevent or lessen seizures by affecting the abnormal electrical activity in the brain.
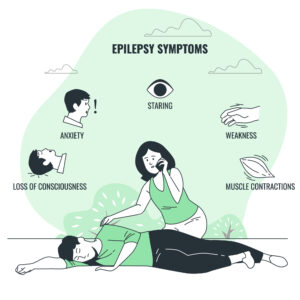
What is epilepsy, and what are the causes of this neurological disorder?
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures. These seizures are caused by abnormal electrical activity in the brain. The exact causes of epilepsy can vary, and they are often classified into two main categories: idiopathic (unknown) causes and symptomatic (identifiable) causes.
- Idiopathic Causes:
- In many cases, the specific cause of epilepsy is unknown. It is believed to result from a combination of genetic and environmental factors. Some individuals may have a genetic predisposition to seizures, but the exact trigger may not be identifiable.
- Symptomatic Causes:
- Epilepsy can also be associated with specific factors or conditions. Common causes include brain injuries, strokes, brain tumors, infections of the brain, and developmental disorders. These identifiable factors contribute to the abnormal electrical activity in the brain, leading to seizures.
It’s important to note that epilepsy can develop at any age, and the causes may vary among individuals. Diagnosing and managing epilepsy typically involve a comprehensive medical evaluation, including medical history, neurological examinations, and diagnostic tests like electroencephalography (EEG).
Understanding the Vagus Nerve and Its Role in Epilepsy:
The vagus nerve, a crucial component of the autonomic nervous system, plays a central role in regulating various bodily functions, such as heart rate, digestion, and respiratory rate. Its intricate connections extend from the brainstem throughout the body, forming a complex network. In the context of epilepsy, the vagus nerve is implicated in the modulation of abnormal electrical activity in the brain, making it a key player in the initiation and propagation of seizures. Understanding the anatomy and function of the vagus nerve lays the foundation for comprehending its critical role in epilepsy and how interventions like Vagus Nerve Stimulation (VNS) can leverage its pathways to bring about therapeutic effects.
In epilepsy, aberrant electrical signals in the brain can lead to seizures, and the vagus nerve’s role in modulating these signals is significant. VNS therapy, a groundbreaking approach, involves the implantation of a device that stimulates the vagus nerve, aiming to influence and regulate neural activity. This neuromodulation, achieved through controlled electrical impulses, forms the basis of VNS’s effectiveness in mitigating the frequency and intensity of seizures. As a result, understanding the vagus nerve’s intricate involvement in epilepsy provides a crucial framework for appreciating how interventions like VNS can harness its potential to bring about positive changes in seizure management.
How VNS Therapy Works to Control Seizures:
Vagus Nerve Stimulation (VNS) therapy operates on the principle of neuromodulation to exert a therapeutic influence on the occurrence and intensity of seizures. This innovative approach involves the implantation of a small device, often likened to a pacemaker, beneath the skin. Connected to the vagus nerve, this device delivers controlled electrical impulses at regular intervals. The targeted stimulation of the vagus nerve then initiates a cascade of effects, influencing neural circuits associated with seizure activity. By modulating abnormal electrical signals in the brain, VNS therapy aims to create a stabilizing impact on the intricate network of neurons, ultimately reducing the propensity for seizures.
The mechanism through which VNS therapy controls seizures is dynamic and adaptive. The implanted device’s electrical impulses are finely tuned to match each patient’s unique neurological profile. These controlled stimulations are designed to interrupt the abnormal neural patterns that contribute to seizures, effectively acting as a regulator for the brain’s electrical activity. As a result, VNS therapy provides a personalized and responsive approach to seizure control, marking a significant departure from traditional antiepileptic medications. This process underscores the potential of VNS therapy as a transformative tool in the management of epilepsy, offering a novel avenue for individuals seeking greater control over their condition.
Is VNS a cure for epilepsy, or does it just manage symptoms?
Vagus Nerve Stimulation (VNS) is not a cure for epilepsy; rather, it is a treatment designed to manage and reduce the frequency and severity of seizures. The goal of VNS is to improve seizure control and enhance the individual’s quality of life. It does not address the underlying cause of epilepsy.
VNS is often considered when other treatments, such as medications, have not provided sufficient seizure control. While it can be highly effective for some individuals, it may not eliminate seizures entirely. Instead, VNS works by delivering regular, mild electrical pulses to the brain through the vagus nerve, helping to modulate abnormal electrical activity and reduce the likelihood of seizures.
It’s important for individuals considering VNS to have realistic expectations and to discuss the potential benefits and limitations of the treatment with their healthcare team. Regular follow-up appointments are typically scheduled to monitor progress, make adjustments to the device settings, and address any concerns or side effects.
Effectiveness of VNS in Seizure Control:
The effectiveness of Vagus Nerve Stimulation (VNS) in seizure control has been substantiated through an array of clinical studies and compelling real-world experiences. Numerous individuals grappling with epilepsy, particularly those resistant to conventional antiepileptic medications, have found a renewed sense of hope and improved quality of life with VNS therapy.
Clinical evidence consistently demonstrates a notable reduction in seizure frequency for a significant proportion of patients who undergo VNS treatment. Success stories underscore the transformative impact, with individuals reporting fewer and less severe seizures, contributing to enhanced daily functioning and a decreased reliance on emergency interventions.
Moreover, VNS has proven to be a viable long-term solution, with sustained efficacy over extended periods, reinforcing its position as a valuable therapeutic option in the comprehensive landscape of epilepsy management. The growing body of evidence supporting the effectiveness of VNS not only attests to its clinical significance but also offers individuals living with epilepsy a tangible and innovative means to regain control over their condition and improve their overall quality of life.
What types of epilepsy are best suited for VNS therapy?
Vagus Nerve Stimulation (VNS) therapy is often considered for individuals with certain types of epilepsy, particularly when other treatments have not been effective. The suitability of VNS can vary, but it is generally considered for the following types:
- Focal Onset Seizures (Partial Seizures): VNS is commonly used for individuals with focal onset seizures, which originate in a specific area of the brain. This type of epilepsy may not fully respond to medications or may be challenging to control with medications alone.
- Drug-Resistant Epilepsy: VNS is often considered when epilepsy is resistant to medications (drug-resistant epilepsy). If multiple medications have been tried without success in controlling seizures, VNS may be a viable option.
- Lennox-Gastaut Syndrome: VNS has been used in individuals with Lennox-Gastaut Syndrome, a severe form of epilepsy that often begins in childhood and is characterized by multiple seizure types.
- Generalized Seizures: While VNS is more commonly associated with focal seizures, it can also be considered for individuals with certain types of generalized seizures, especially if other treatments have not been effective.
It’s important to note that the decision to use VNS is based on an individual’s specific case and their response to other treatments. A healthcare professional, typically a neurologist or epileptologist, will assess the person’s medical history, seizure types, and treatment history to determine whether VNS is a suitable option.
The effectiveness of VNS can vary from person to person, and not everyone with epilepsy will be a candidate for or benefit from VNS therapy. If considering VNS, it’s essential to have a thorough discussion with a healthcare provider to assess the potential benefits and risks based on individual circumstances.
Can VNS be used in conjunction with other epilepsy treatments, such as medications or surgery?
Yes, Vagus Nerve Stimulation (VNS) can be used in conjunction with other epilepsy treatments, including medications or surgery. In fact, it is not uncommon for individuals with epilepsy to undergo a combination of treatments to achieve better seizure control. Here are some scenarios where VNS might be used alongside other interventions:
- Adjunct to Medications: VNS is often considered when epilepsy is resistant to medications, meaning that seizures persist despite trying multiple anti-seizure medications. In such cases, VNS can be added as an adjunctive therapy to complement the effects of medications.
- Complementary to Surgery: For individuals with certain types of epilepsy that are focal and originate from a specific area of the brain, surgical options may be considered. In some cases, VNS may be used either before or after surgery, or in conjunction with surgery, to enhance seizure control.
- Combined Approaches for Complex Cases: In cases of complex or refractory epilepsy where seizures are difficult to control, healthcare providers may recommend a combination of treatments. This could involve using VNS along with medications, lifestyle modifications, and other therapeutic approaches.
- Individualized Treatment Plans: The choice of treatments, including VNS, is highly individualized. Healthcare providers consider factors such as the type of epilepsy, seizure frequency, response to medications, and the overall health of the individual when developing a treatment plan.
Individuals with epilepsy need to work closely with their healthcare team to discuss the potential benefits and risks of combining treatments.
What is the success rate of VNS in reducing seizures, and are there any long-term considerations?
The success rate of Vagus Nerve Stimulation (VNS) in reducing seizures can vary among individuals. While some people experience significant improvement, others may see more modest results. It’s important to note that VNS is not a cure for epilepsy, and the goal is often to reduce the frequency and severity of seizures rather than eliminate them entirely.
The effectiveness of VNS tends to become more apparent over time, and the response to treatment can vary. In general, the success rate is influenced by factors such as the individual’s specific type of epilepsy, the duration and severity of their condition, and how well they respond to VNS therapy.
Long-term considerations for VNS therapy include:
- Adjustments and Optimization: VNS devices are programmable, and the settings can be adjusted over time to find the optimal level of stimulation for each individual. Regular follow-up appointments with healthcare providers are essential for monitoring progress and making any necessary adjustments.
- Maintenance and Monitoring: Routine maintenance of the VNS device may be necessary, and regular check-ups are typically scheduled to ensure that the device is functioning correctly. Monitoring for any changes in seizure patterns or side effects is also part of the long-term care plan.
- Battery Replacement: The VNS device has a battery that may need to be replaced after several years, depending on usage. This is typically done through a minor surgical procedure.
- Lifestyle Considerations: Individuals with VNS devices may need to make certain lifestyle adjustments. For example, certain activities or settings may need to be avoided due to the potential impact on the VNS device.
- Commitment to Follow-Up Care: Long-term success with VNS often requires a commitment to ongoing follow-up care with healthcare providers. This includes communication about any changes in seizure activity, side effects, or other concerns.
It’s important for individuals considering VNS to discuss the potential benefits and long-term considerations with their healthcare team. Each person’s experience with VNS is unique, and a collaborative approach between the individual and their healthcare providers is crucial for optimizing treatment outcomes over the long term.
Conclusion
In conclusion, Vagus Nerve Stimulation therapy stands as a game-changer in the landscape of epilepsy treatment, offering transformative hope for those seeking effective seizure control. Its dynamic interplay with the vagus nerve, coupled with personalized neuromodulation, paints a picture of a future where individuals can reclaim agency over their lives despite the challenges posed by epilepsy. As research and technology continue to advance, the potential for further innovations in epilepsy management remains bright, promising continued progress in enhancing the lives of those affected by this complex neurological condition.
If you need more information, please feel free to contact us.


